Diabetes is Rising — Are We Prepared?
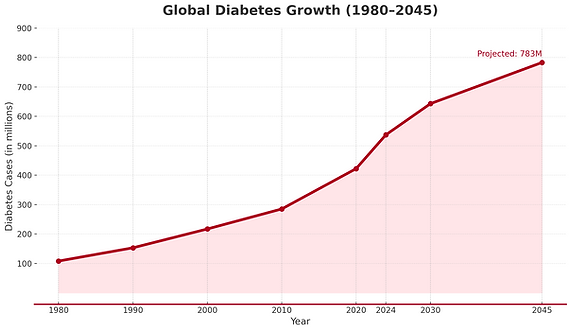
537m
are living with diabetes right now
643m
adults predicted to have diabetes by 2030
783m
adults predicted to have diabetes by 2045
Every 5 seconds, someone is diagnosed. Many remain undiagnosed until complications arise. But what if we could detect risks early and empower individuals to take control?

Source: The World Bank 2021, IDF Atlas 10th edition. Image retrieved from www.visualcapitalist.com. For illustrative purposes only.
The Numbers Behind the Crisis
Diabetes cases have quadrupled in the last 40 years. What was once a manageable disease now places immence strain on healthcare systems and individuals alike.
1 in 10 Americans
has diabetes, and nearly 100 million more have prediabetes—81% don’t even know it (American Diabetes Association, 2024).
50% more likely to develop diabetes
Black & Hispanic/Latino individuals are 50% more likely to develop diabetes than non-Hispanic White individuals (ADA, 2024).
8th leading cause of death
In 2021, diabetes was the 8th leading cause of death in the U.S., contributing to 103,000 deaths (CDC, 2024).
2.6 times higher medical costs
Medical costs for diabetes patients are 2.6 times higher than those without it, reaching a staggering $412.9 billion annually (ADA, 2024).
Why Are So Many People Developing Diabetes?
The root causes of diabetes are deeply intertwined with modern lifestyles, economic factors, and systemic healthcare gaps
Ultra-processed diets
and high sugar consumption fuel insulin resistance.
Sedentary lifestyles
and desk jobs reduce physical activity, worsening metabolic health
Obesity epidemic
nearly 80% of Type 2 diabetes cases are linked to excess weight.
Social & economic barriers
limit access to nutritious food, preventive care, and medications
Environmental disruptors
like pollution and endocrine disruptors (BPA, microplastics) interfere with insulin regulation.
Why the Challenges Persist: Barriers to Better Diabetes Care
The root causes of diabetes are deeply intertwined with modern lifestyles, economic factors, and systemic healthcare gaps
High Treatment Costs
Insulin prices have surged, making medication unaffordable for many.
Healthcare Disparities
Low-income communities have higher diabetes rates but fewer resources for proper management.
Lack of Education & Support
Many patients don’t receive proper diabetes self-management training, leading to complications.
Food Insecurity & Lifestyle Habits
Unhealthy food is often more affordable and accessible than fresh, nutritious options.
Fragmented Care Systems
Poor coordination between healthcare providers leads to delayed treatments.

Source: World Heart Federation, via ResearchGate.
How Health Jeanie is changing Diabetes Care
Traditional diabetes care is often reactive—waiting for symptoms to worsen before taking action. Health Jeanie transforms this approach with AI-powered precision:
Early Risk Detection
AI analyses patient data to identify warning signs before complications arise.
Personalized Health Plans
Adaptive interventions tailored to individual lifestyles, risk factors, and needs.
Managing comorbidities
Jeanie helps reduce the impact of diabetes on quality of life and cost
Nutrition and Diet
Jeanie helps track nutrition very easily by simply taking picture of food and provides diet insights
24/7 Guidance & Alerts
Real-time tracking of glucose levels, medications, and adherence trends.

Key Trends in Diabetes Prevention & Management
As diabetes rates rise, the healthcare industry is shifting focus toward smarter prevention and personalized intervention.
01
AI-Driven Risk Prediction
AI can identify comorbidities, and at-risk individuals early, enabling preventive care before diabetes develops.
02
Wearable Technology
Continuous glucose monitors (CGMs) help patients track blood sugar levels in real time.
03
Expanding Access to Affordable Medications
Initiatives like price caps on insulin are reducing financial strain.
04
Addressing Social Determinants of Health (SDoH)
Health organizations are focusing on food security, healthcare access, and financial stability as key factors in diabetes care.
05
Diet, nutrition, and lifestyle
Personalized nutrition, physical activity, and lifestyle coaching are being prioritized to help patients manage and improve long-term health outcomes.
